Pelvic Organ Prolapse And Pelvic Health Physiotherapy
One in three women are affected by significant pelvic organ prolapse.
Do you have a feeling of heaviness or dragging, or a lump or bulge in your vagina?
Has your GP told you that you have prolapse?
Pelvic Health Physiotherapy can help.

What is pelvic organ prolapse?
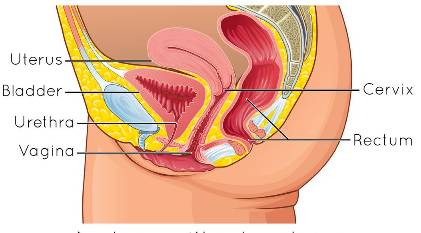
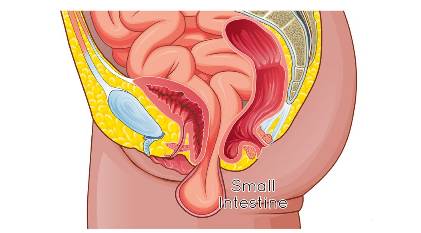
The organs in your pelvis are your uterus, bladder and bowel. These organs are held within the pelvis by your ligaments, connective tissue and pelvic floor muscles.
If these supporting tissues become stretched, torn or weak, any of your pelvic organs can shift in position. One or all of these organs can then bulge down into the vagina. This can feel irritating and may impact on your quality of life.
Common symptoms of pelvic organ prolapse
Early on, you may not know that you have prolapse. Your doctor or nurse may mention that you have some prolapse at a routine pap smear.
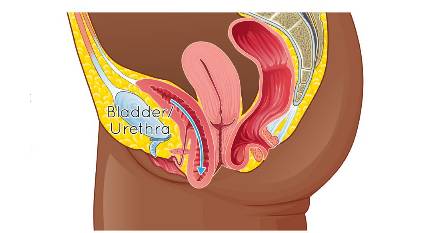
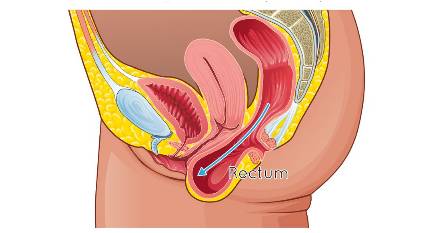
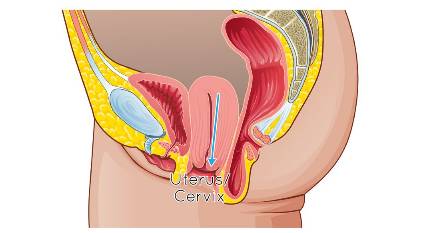
If the pelvic organ drops down further you might notice the following symptoms:
- A bulge at the entrance to your vagina
- A feeling of heaviness or dragging in your vagina or pelvis, especially at the end of the dayor after doing activities such as heavy lifting
- Difficulty emptying your bladder or bowel
- Recurrent urinary tract infections
- Sexual problems, including pain with intercourse and concerns about the impact of the prolapse on intimacy
- Lower back pain
- Not being able to enjoy general exercise
Possible causes of pelvic organ prolapse
The pelvic organs are held in place by supportive ligaments and connective tissues inside the pelvis, as well as the pelvic floor muscles below. Anything that causes damage or weakness to these supportive tissues can contribute to prolapse, such as the following:
Pelvic floor muscles can become weak through lack of use and through other factors mentioned below
Pregnancy and vaginal delivery both stretch the pelvic ligaments and connective tissues, as well as the pelvic floor muscles.
Lifting heavy items may increase pressure in the abdomen, causing the pelvic support tissues to stretch.
Prolonged coughing puts pressure on the pelvic organ support system.
Being overweight puts an extra load on the pelvic organ support system. 70% of women with obesity have pelvic organ prolapse.
Straining your muscles due to constipation can weaken the pelvic floor muscles.
Pelvic floor muscles lose strength with age, particularly as a result of menopause.
Prolapse tends to run in families.
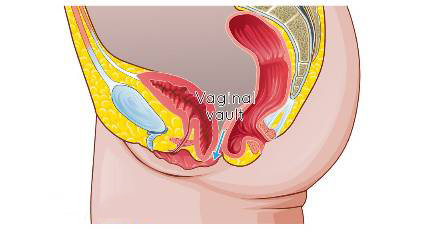
Prolapse can occur in women who have had a hysterectomy. In this case, the top of the vagina moves down into the vaginal canal.

Management of pelvic organ prolapse
Management of pelvic organ prolapse can be conservative or surgical. The aim of treatment is to eliminate the symptoms associated with the prolapse.
Conservative management
Conservative management occurs with a Pelvic Health Physiotherapist. A Pelvic Health Physiotherapist is a physiotherapist with extra qualifications and a special interest in Pelvic Health. They are best equipped to assess, treat and rehabilitate prolapse. Research shows that you can reduce prolapse symptoms and stop the prolapse getting worse through a personalised exercise program.
Conservative management involves the following:
Lifestyle advice
After considering possible causes of prolapse, your Pelvic Health Physiotherapist will give you information and advice about lifestyle changes you can make to manage your prolapse. This may involve information about general exercise (what is helpful versus unhelpful),
reducing body weight, or encouragement to see your GP about an ongoing cough. You will also be educated about good bladder and bowel habits, as this will also help to manage your prolapse.
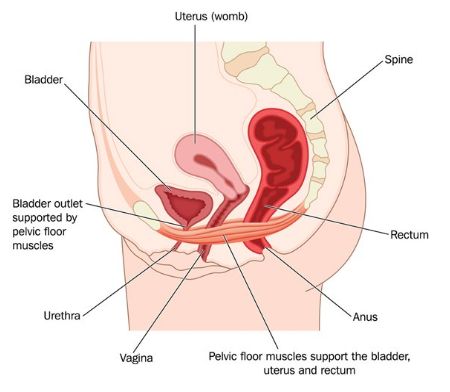

Pelvic floor muscle training
Your pelvic floor muscles are the muscles at the base of your pelvis. They attach from the pubic bone at the front to the tailbone at the back and also from side to side. These are the muscles that help support your pelvic organs. Your physiotherapist will assess your pelvic floor muscles through vaginal examination and/or by using a real-time ultrasound. They will evaluate the function of your pelvic floor muscles and assess whether you are able to contract and relax these muscles. You will learn how to exercise these muscles correctly and will be given a home program of exercises if required.
The real-time ultrasound gives you immediate visual feedback so you will be able see when you are contracting and relaxing your pelvic floor muscles. This will help you to be confident that you are doing your exercises properly.
Symptom management
Depending on the type of prolapse you have, you may benefit from advice to help you empty your bladder and bowel more effectively, or to help you to have pain-free sexual intercourse.
Vaginal support pessary
In consultation with your doctor, a vaginal support pessary may be prescribed by your Pelvic Health Physiotherapist. A vaginal support pessary is a silicon device that can be fitted into the vagina to provide support to the pelvic organs and therefore relieve your symptoms. These must be fitted by someone who has had training in fitting vaginal support pessaries.

General exercise advice
Maintaining your general fitness will help improve overall muscle tone in your body, including your pelvic floor. Daily physical activity will also keep your bowel regular. Your Pelvic Health Physiotherapist will help you establish an exercise program, taking into account your individual goals and preferred exercise.
Surgical management
Surgery can be performed by a specialist to repair torn or stretched ligaments and connective tissues. Surgery may be considered if conservative measures have failed or if the prolapse is severe.
Your Pelvic Health team at Southern Coast Pelvic Health
All physiotherapists at Southern Coast Pelvic Health have a special interest and training in Pelvic Health.
Conditions that our Pelvic Health Physiotherapists treat include:
- Stress urinary incontinence
- Urge urinary incontinence and urinary urgency
- Urinary frequency and nocturia
- Pelvic organ prolapse
- Post-prostate surgery management
- Post-gynaecological surgery management
- Bowel dysfunction including constipation, faecal urgency and faecal incontinence
- Pre- and post-natal care, including pregnancy-related pelvic girdle pain, abdominal separationand mastitis
- Pelvic pain including vaginismus, dyspareunia and chronic pelvic pain.
Who else can help?
General Practitioner (GP): Your local GP can refer you for any tests required, prescribe medication and refer you to a Pelvic Health Physiotherapist or specialist if needed.
Urologist or Gynaecologist: These specialists may refer you for investigations, prescribe medication or refer you to a Pelvic Health Physiotherapist. They may also discuss surgical options.