Pelvic Health Physiotherapy Following Prostate Surgery
Are you aware that loss of bladder control often occurs after prostate surgery?
Did you know that pelvic floor muscle exercises can help resolve this?
Pelvic Health Physiotherapy can help.
Many men have problems with bladder control following prostate surgery. For some, it is the most challenging thing to deal with following the surgery, particularly if they haven’t had problems with incontinence before.

What Is Urinary Incontinence?
Urinary incontinence is any accidental loss of urine. It can vary from a few drops to a large amount of urine. It usually occurs with coughing, changing direction, exercise or physical activity.
Why does urinary incontinence occur after prostate surgery?
When the prostate is removed, damage can occur to one of the sphincters that controls the bladder. Our pelvic floor muscles, which also help bladder control, then need to work exceptionally well to compensate for this. If the pelvic floor muscles aren’t functioning optimally, leakage of urine can occur.
How Severe Will The Incontinence Be?
What can be done to treat the incontinence?
Conservative management of urinary incontinence is done by a pelvic health physiotherapist. A pelvic health physiotherapist is a physiotherapist with extra qualifications and a special interest in pelvic health. They are best equipped to assess, treat and manage urinary incontinence following prostate surgery A pelvic health physiotherapist is likely to advise you to:
It is important to have a rest in the afternoon while recuperating, particularly in the first 2 weeks after your operation. Your pelvic floor muscles need to work hard and will need time to recover each day. If a particular activity or exercise causes urine to leak, avoid that activity for a while.
Do pelvic floor muscle exercises
Performing pelvic floor exercises after prostate surgery is vital to your recovery. You can start these after your catheter comes out.
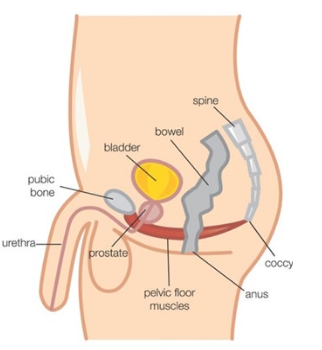
Your pelvic floor muscles are the muscles at the base of your pelvis. They attach from the pubic bone at the front to the tailbone at the back and from side to side. These are the muscles that help control the bladder and bowel. Activating these muscles involves squeezing and drawing in around the anus as if stopping the flow of urine. You should feel closure around the anus and urethra. You don’t need to tighten your buttocks or abdominal muscles.
Real-time ultrasound gives you immediate visual feedback so you will be able see when you are contracting and relaxing your pelvic floor muscles. This will help you to be confident that you are doing your exercises properly.
Commence bladder re-training

After having the catheter in you may find that you do not experience a normal feeling of bladder fullness. It is important to practice holding on for longer to increase the amount of urine in the bladder. Your Pelvic Health Physiotherapist may want you to keep a bladder diary to assist in monitoring this.
Drink Well
It is best to drink 1.5–2 litres of fluid per day, mostly water. Avoid caffeine, alcohol and fizzy drinks because they can irritate your bladder.
Practise good toilet habits
Your Pelvic Health Physiotherapist may ask you to fill in bladder and bowel diaries. This allows the physiotherapist to see how your bladder and bowel are functioning, so they can give advice accordingly.
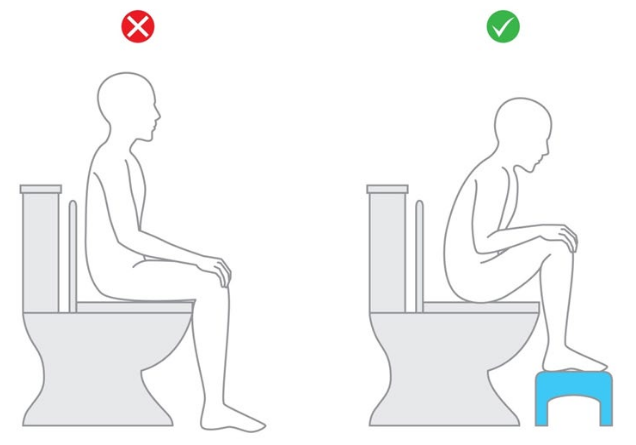
Sit on the toilet with correct posture to help prevent bladder and bowel problems.
Exercise
Maintaining your general fitness will help improve the overall muscle tone in your body, including your pelvic floor. Daily physical activity will also keep your bowel regular. Your Pelvic Health Physiotherapist will help you establish an exercise program, taking into account your individual goals and preferred exercise.
How Often Will I Need To See The Pelvic Health Physiotherapist?
Ideally you will see your Pelvic Health Physiotherapist once or twice before the surgery. This allows the physiotherapist to do a thorough assessment and teach you how to exercise your pelvic floor muscles correctly. This is easier to do before the surgery. They may also ask you to keep some bladder and bowel diaries, to see how your bladder and bowel are working before the surgery.
After the surgery, the number of appointments will depend on the severity of the leakage and your improvement in symptoms. Your Pelvic Health Physiotherapist will liaise closely with your specialist regarding your progress.
Your Pelvic Health Team At Southern Coast Pelvic Health
All physiotherapists at Southern Coast Pelvic Health have a special interest and training in Pelvic Health.
Conditions that our Pelvic Health Physiotherapists treat include:
- Stress urinary incontinence
- Urge urinary incontinence and urinary urgency
- Urinary frequency and nocturia
- Pelvic organ prolapse
- Post-prostate surgery management
- Post-gynaecological surgery management
- Bowel dysfunction including constipation, faecal urgency and faecal incontinence
- Pre- and post-natal care, including pregnancyrelated pelvic girdle pain, abdominal separation and mastitis
- Pelvic pain including vaginismus, dyspareunia
- and chronic pelvic pain.

Who Else Can Help?
Continence nurse advisor: Your continence nurse advisor can inform you about continence treatment and continence aids such as pads.
General Practitioner (GP): Your local GP can refer you to you for any tests required to prescribe medication and refer you to a Pelvic Health Physiotherapist.
Urologist and Oncologist: These specialists may refer you for investigations, prescribe medication or refer you to a Pelvic Health Physiotherapist. They may also discuss surgical options.
