Urinary Incontinence And Pelvic Health Physiotherapy
Do you leak urine when you cough, sneeze, laugh or exercise?
Do you have to rush to the toilet to urinate?
These are symptoms of urinary incontinence.
Pelvic Health Physiotherapy can help.
Urinary incontinence affects 5 million people in Australia, both men and women. The great news is that it can be treated and in many cases cured.

What Is Urinary Incontinence?
Urinary incontinence is any accidental loss of urine. It can vary from a few drops of urine to a full emptying of the bladder.
What other symptoms may occur with urinary incontinence?
Urgency: having an urgent desire to urinate
Frequency: urinating more often than usual
Nocturia: waking more than once a night to urinate
Nocturnal enuresis: leaking urine while asleep
What Are The Types Of Urinary Incontinence?
- Stress incontinence: leaking urine when coughing, sneezing, laughing, lifting or doing exercise
- Urge incontinence: feeling urgency to rush to the toilet, with some urine leaking
- Incontinence associated with chronic retention: when the bladder is not able to empty properly, frequent small amounts of urine may leak
- Functional incontinence: leaking

What Are Some Of The Causes Of Urinary Incontinence?
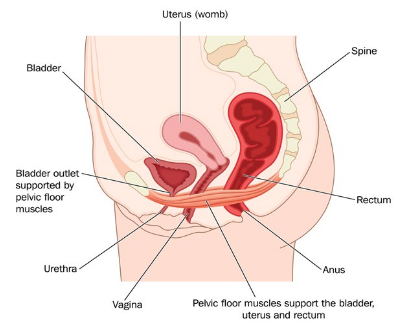
- Weak pelvic floor muscles from constipation, chronic coughing, being overweight, pregnancy, vaginal birth delivery, or heavy lifting.
- Menopause in women: The reduction in oestrogen that occurs during menopause can result in thinning of the urethra. Urine may leak if the urethra does not close as well as it used to.
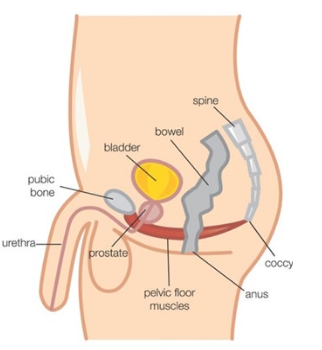
- Prostate surgery in men: Many men experience urinary incontinence after prostate surgery.
- Urinary tract infections sometimes cause urine to leak.
- Poor drinking habits: Different types and amounts of fluid can irritate the bladder and cause incontinence.
- Poor toilet habits: Going to the toilet “just in case” trains the bladder to store smaller volumes than it should, which can cause incontinence.
- Conditions such as Parkinson’s disease, multiple sclerosis, stroke and diabetes can interfere with bladder sensations and emptying.
- Anatomical problems can block the urethra, e.g. enlarged prostate, pressure from a full rectum, bladder stones or other growths.
- Some medications can affect bladder function, e.g. diuretics make the bladder produce urine more quickly, increasing urgency.Weak pelvic floor muscles from constipation, chronic coughing, being overweight,pregnancy, vaginal birth delivery, or heavy lifting.
Pelvic Health Physiotherapy Assessment For Urinary Incontinence
- A comprehensive history will be taken so we can understand your main concerns, what might be contributing to them and your goals for treatment
- You may be asked to complete some questionnaires and bladder and bowel diaries
- Your Pelvic Health Physiotherapist will do a physical assessment of your pelvic floor muscles. They may use the real-time ultrasound as part of this assessment. They will evaluate the function of your pelvic floor muscles and assess your ability to contract and relax these muscles. Some people think that their pelvic floor muscles are weak and stretched, while the opposite may be the case. For some people the pelvic floor muscles are too active and they will need to be taught to relax these muscles. You will learn how to exercise your pelvic floor muscles according to what is needed for you.

Real-time ultrasound gives you immediate visual feedback so you will be able see when you are contracting and relaxing the pelvic floor muscles. This will help you to be confident that you are doing your exercises properly.
You can also talk to your doctor about urinary incontinence. There are a variety of tests that your doctor may recommend, including analysis of a urine sample, an ultrasound or a urodynamic study.
Management Of Urinary Incontinence
Management of urinary incontinence can be through conservative treatment, medicines or surgery. Initial treatment should be conservative; this is done with a Pelvic Health Physiotherapist.
Conservative Management
A Pelvic Health Physiotherapist is a physiotherapist with extra qualifications and a special interest in pelvic health. They are best equipped to assess, treat and manage urinary incontinence.
Conservative Management May Involve:
Lifestyle advice
After considering possible causes of urinary incontinence, your Pelvic Health Physiotherapist will give you advice on lifestyle changes you can make to help manage your incontinence.
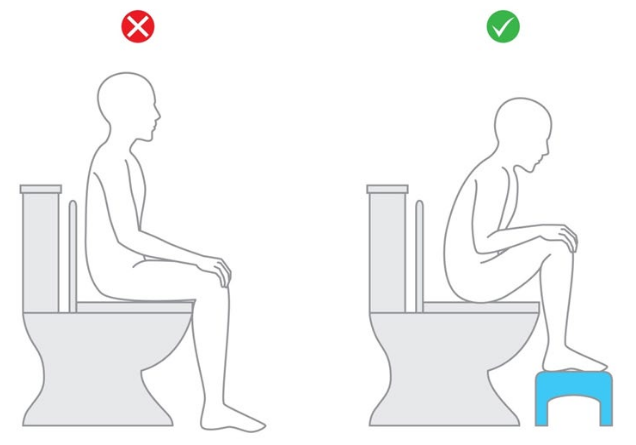
The discussion may include information about general exercise (what is helpful versus unhelpful), education about reducing your body weight or encouragement to see your GP about an ongoing cough. You will be educated about good bladder and bowel habits. You will be advised to sit on the toilet with correct posture.
Behaviour Re-training And Bladder Retraining
People with urge incontinence need to learn urge suppression and control techniques to reduce the sensation of urgency. They may also need to void at certain intervals to train the bladder to give correct signals of fullness. Your bladder diary will help to determine if bladder re-training is necessary.
Pelvic Floor Muscle Training
Your pelvic floor muscles are the muscles at the base of your pelvis. They attach from the pubic bone at the front to the tailbone at the back and from side to side. These are the muscles that help maintain continence and support your pelvic organs.
To activate your pelvic floor muscles, squeeze and draw in as if stopping the flow of urine. You should feel closure around the anus and urethra. Women will feel this in the vagina also. You don’t need to tighten your buttocks or abdominal muscles.
Once you have mastered this muscle activation with the guidance of your Pelvic Health Physiotherapist, they will design you a pelvic floor muscle training program. The program will be reviewed and changed during subsequent treatment sessions. It takes time to alter the pelvic floor muscles and improve their function.
© Continence Foundation of Australia
Other Physiotherapy Treatments
Depending on the type of urinary incontinence you are experiencing, your Pelvic Health Physiotherapist may recommend that you use weights, support pessaries, electrical stimulation or biofeedback, in addition to your other methods of management.
General Exercise Advice
Maintaining your general fitness will help improve overall muscle tone in your body, including your pelvic floor. Daily physical activity will also keep your bowel emptying at regular intervals. Your Pelvic Health Physiotherapist will help you establish an exercise program, taking into account your individual goals and preferred exercise.
Medical And Surgical Management
Your doctor will advise you if medications or surgery are appropriate. Medications help with some forms of urinary incontinence. Injectable agents or surgery may be considered if conservative measures have failed or if the incontinence is severe.
Your Pelvic Health Team At Southern Coast Pelvic Health
All physiotherapists at Southern Coast Pelvic Health have a special interest and training in Pelvic Health.
Conditions that our Pelvic Health physiotherapists treat include:
- Stress urinary incontinence
- Urge urinary incontinence and urinary urgency
- Urinary frequency and nocturia
- Pelvic organ prolapse
- Post-prostate surgery management
- Post-gynaecological surgery management
- Bowel dysfunction including constipation, faecal urgency and faecal incontinence
- Pre- and post-natal care, including pregnancy-related pelvic girdle pain, abdominal separation and mastitis
- Pelvic pain including vaginismus, dyspareunia and chronic pelvic pain.
Who Else Can Help?
Continence nurse advisor: Your continence nurse advisor can inform you about continence treatment and continence aids such as pads.
General Practitioner (GP): Your local GP can refer you for any tests required to prescribe medication and refer you to a Pelvic Health Physiotherapist or specialist if required.
Urologist or Gynaecologist: These specialists may refer you for investigations, prescribe medication or refer you to a Pelvic Health Physiotherapist. They may also discuss surgical options.

